About SUDOSCAN
The Advantage of Neuropathy Early Detection
An innovative device for early detection and follow-up of Autonomic and Small Fiber Neuropathy.
Simple results obtained in 3 minutes.
3 Minutes
Simple
QUANTITATIVE
Non-Invasive
Objective
THE SCIENCE
Early identification and follow-up of peripheral automatic neuropathies
• Establish diagnosis
• Control effectiveness of treatment
• Provide quantitative data to adapt patient care and lifestyle.

Why test sweat gland function?
Sweat glands are innervated by small sympathetic C-fibers. Sudomotor (sweat) dysfunction can be one of the earliest detectable neurophysiologic abnormalities in distal small fiber neuropathies. Quantitative assessment of sweat response has been proposed as an index of the severity of autonomic failure as well as an early indicator for regeneration of small fibers [1,2,3].
Diabetes has been shown to be the most common identifiable cause of small fiber neuropathy. The American Diabetes Association (ADA) has identified sudomotor (sweat) dysfunction as one of the major clinical manifestations of diabetic autonomic neuropathy. Furthermore, the assessment of autonomic dysfunction may identify patients at high risk for cardiac autonomic neuropathy, which carries a very high rate of morbidity and mortality [4].
What are the alternatives ?
The use of skin biopsy to measure Intraepidermal Nerve Fiber Density (IENFD) or Sweat Gland Nerve Fiber Density (SGNFD) is an accepted surrogate measure of small fiber neuropathy. While skin biopsy is well accepted by the medical community, it has certain limitations as: invasiveness, risk of infection, bleeding, and a limited number of laboratories that can process the
sample [6]. The Quantitative Sudomotor Axon Reflex Test (QSART) measures sweat response under controlled humidity and temperature conditions. It requires fairly expensive equipment and is available in few centers.
THE PRINCIPLE
How does it work?
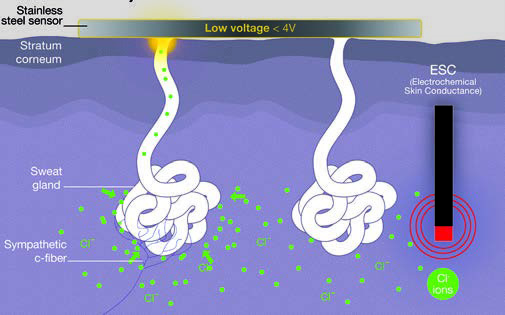
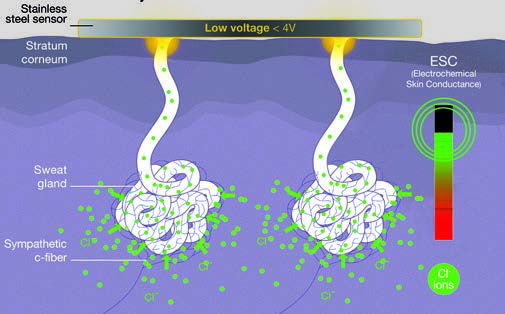
The degeneration of small nerve fibers reduces sweat gland innervation and alters sudomotor function [7]. Sudoscan measures the concentration of chloride ions produced by sweat gland activity.
A low-voltage current (<4V) is applied to the hands and feet through stainless steel sensor electrodes. The applied tension extracts chloride ions from the sweat glands which are densely concentrated on the palms and soles. Since the stratum corneum acts as an isolator, the ions can only pass via the sweat ducts. This ensures that the findings correspond solely to sweat gland function. The chloride ions create a detectable electrochemical reaction with the sensor plates which is measured.
What is measured
SUDOSCAN records the Electrochemical Skin Conductances (ESC) of the hands and feet generated from the current associated with the applied voltage. Loss of sweat glands or loss of their innervations results in reduced ESC [8].
THE SOLUTION

SUDOSCAN at a glance
- Fast
- No patient preparation
- Results in 3 minutes
- Automatic reports
Simple
- Non-invasive
- No fasting necessary
- Easy training
- Touch screen operation
Accurate
- Quantitative results
- Proven clinical results
- Operator independent
- Four hands and feet electrodes
- Automatic quality check
Fast testing
SUDOSCAN provides an accurate evaluation of sudomotor function by measuring the ability of sweat glands to release chloride ions in response to an electrochemical activation on the palm of the hands and soles of the feet, areas with the highest sweat gland density [9] in less than 3 minutes.
Clear results
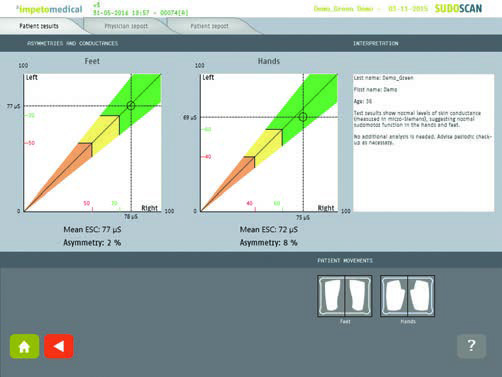
1 Simple
Ergonomic touch screen operation and detailed graphics allow for visual representation of the results. An immediate quality check ensures reliable results. Results are easy to interpret : Green suggests no neuropathy, Yellow a moderate neuropathy and Orange a more severe neuropathy.
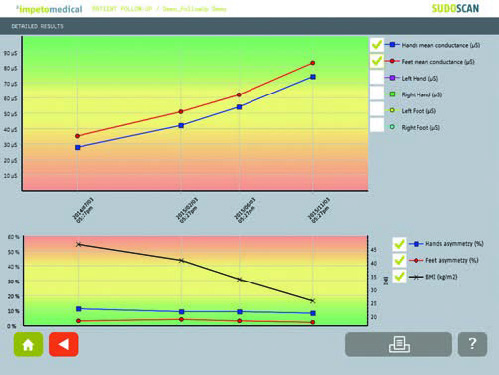
2 Quantitative
Actual numerical values of the Electrochemical Skin Conductance (ESC) of each hand and foot are displayed. The level of ESC indicates the severity of the neuropathy. This measure can be compared with later test results to assess the patient’s response to treatment or other prescribed interventions or the evolution of the neuropathy.
3 Accurate
Measure of symmetry between right and left sides help identify the type of peripheral neuropathy.
THE APPLICATION
A broad range of diseases
Sudomotor dysfunction is a common finding, and one of the earliest detectable abnormalities in a number of peripheral and autonomic neuropathies.
SUDOSCAN has been tested for small fiber nerve neuropathies in several diseases and compared to guidelines reference tests:
- Diabetes
- Parkinson
- Chemotherapy induced polyneuropathy
- Familial amyloid polyneuropathy
- Fabry disease

The advantage of Neuropathy Early Detection
An innovative device for early detection and follow-up of Autonomic and Small Fiber Neuropathy.
Simple results obtained in 3 minutes.
SUDOSCAN Benefits
Fast
No patient preparation
Results in 3 minutes
Easy-to-read critical data points to help physicians reach a diagnosis
Secure
No fasting
Easy to operate
CE and FDA approvals
TGA and Medsafe approved
Accurate
Independent from environmental conditions
Backed by evidence-based research
150 peer-reviewed journals publications
References
[1] Illigens et al. Sweat testing to evaluate autonomic function. Clinical Autonomic Research. 2008;19(2):79-87
[2] Low PA. Evaluation of sudomotor function. Clinical Neurophysiology. 2004;115(7):1506-1513.
[3] Gibbons et al. Capsaicin induces degeneration of cutaneous autonomic nerve fibers. Annals of Neurology. 2010;68(6):888-898.
[4] Tesfaye et al. Diabetic neuropathies: update on definitions, diagnostic criteria, estimation of severity, and treatments. Diabetes Care. 2010;33(10):2285-2293.
[5] Vinik et al. Diabetic neuropathies: clinical manifestations and current treatment options. Nature Clinical Practice Endocrinology & Metabolism. 2006;2:269-281.
[6] Joint Task Force of the EFNS and the PNS. European Federation of Neurological Societies/Peripheral Nerve Society Guideline on the use of skin biopsy in the diagnosis of small fiber neuropathy. Report of a joint task force of the European Federation of Neurological Societies and the Peripheral Nerve Society. Journal of the Peripheral Nervous System. 2010;15(2):79-92.
[7] Smith et al. SUDOSCAN as a Diagnostic Tool for Peripheral Neuropathy. Peripheral Nerve Society poster, Saint-Malo. June 2013.
[8] Ayoub et al. Electrochemical Characterization of Nickel Electrodes in Phosphate and Carbonate Electrolytes in View of Assessing a Medical Diagnostic Device for the Detection of Early Diabetes. Electroanalysis. 2010;21:2483-2490.
[9] Hubert et al. Abnormal electrochemical skin conductance in cystic fibrosis. Journal of cystic fibrosis. 2010;10(1):15-20.
[10] Vinik et al. SUDOSCAN, a non-invasive tool for detecting diabetic small fiber neuropathy and autonomic dysfunction. Diabetes technology and therapeutics. 2013;15(11).
[11] Selvarajah et al. SUDOSCAN: A Simple, Rapid, and Objective Method with Potential for Screening for Diabetic Peripheral Neuropathy. PLoS One. 2015 Oct 12;10(10):e0138224.
[12] Schwarz et al. Assessment of Small Fiber Neuropathy through a Quick, Simple and Non Invasive Method in a German Diabetes Outpatient Clinic. Experimental and Clinical
Endocrinology & Diabetes. 2013;121(2):80-83.
[13] Raisanen et al. Sudomotor Function as a tool for Cardiorespiratory Fitness Level Education: Comparison with Maximal Exercice Capacity. International Journal of Environmental Research and Public Health. 2014;11(6):5839-5848.
[14] Smith et al. The diagnostic utility of Sudoscan for distal symmetric peripheral neuropathy. Journal of Diabetes and its Complications. 2014;28(4):511-516.
[15] Saad et al. Quick, non-invasive and quantitative assessment of small fiber neuropathy in patients receiving chemotherapy. Journal of Neuro-Oncology. 2016;127(2):373-380.
[16] Lefaucheur et al. Diagnosis of small fiber neuropathy: A comparative study of five neurophysiological tests. Neurophysiologie Clinique/Clinical Neurophysiology. 2015;45(6):445-455.
[17] Obici et al. Recommendations for presymptomatic genetic testing and management of individuals at risk for hereditary transthyretin amyloidosis. Current Opinion in Neurology. 2016;29:S27-S35.
[18] Castro et al. The diagnostic accuracy of Sudoscan in transthyretin familial amyloid polyneuropathy. Clinical Neurophysiology. 2016;127(5):2222-2227.



